Femoroacetabular Impingement (FAI) is a motion-related disorder of the hip joint that can significantly affect mobility, especially in young athletes and active adults. This condition arises when abnormal contact between the femoral head and the acetabular rim leads to joint damage, pain, and restricted movement.
In this blog, we’ll explore:
- What is Femoroacetabular Impingement?
- Primary causes of FAI
- Secondary causes of FAI
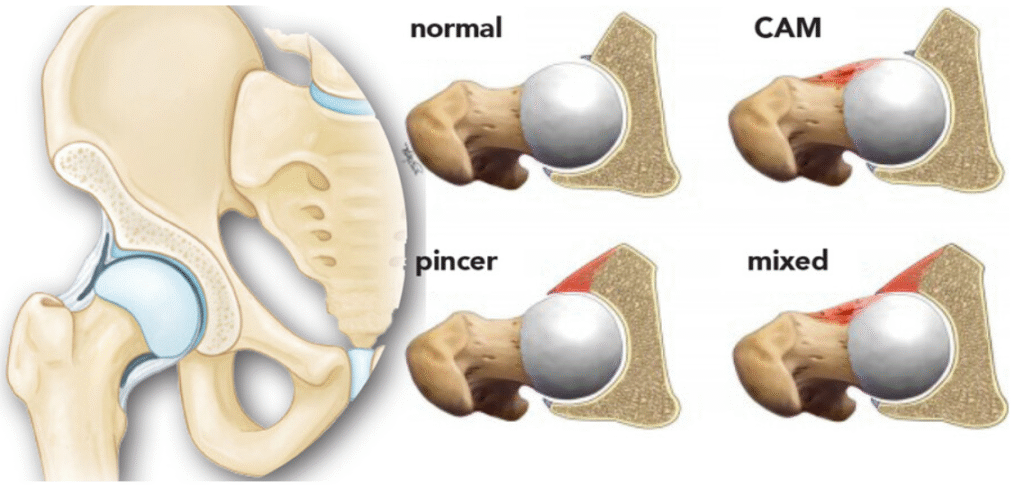
- Types of FAI: Cam, Pincer, and Mixed
- Symptoms and diagnosis
- Physiotherapy management of FAI
- When to consider surgical referral
🔍 What Is Femoroacetabular Impingement (FAI)?
Femoroacetabular Impingement (FAI) is a condition where the bones of the hip joint—specifically the femoral head and the acetabulum—do not fit together properly. This mismatch leads to abnormal friction during hip movements, especially flexion and rotation, causing damage to the labrum and articular cartilage over time.

🧬 Primary Causes of Femoroacetabular Impingement
Primary causes are typically idiopathic or developmental in nature, meaning they arise without a specific injury or disease. These include:
1. Cam Morphology
- Occurs when the femoral head is not perfectly round.
- Leads to abnormal contact with the acetabulum during hip flexion.
- Common in young athletic males.
2. Pincer Morphology
- Results from acetabular overcoverage.
- The acetabular rim extends too far, compressing the labrum.
- More common in middle-aged women.
3. Combined (Mixed) Morphology
- A combination of cam and pincer features.
- Seen in approximately 85% of symptomatic FAI cases.
4. Genetic and Growth Factors
- Abnormal bone development during adolescence.
- High-impact sports during skeletal maturation (e.g., football, hockey, gymnastics).
🧠 Secondary Causes of Femoroacetabular Impingement
Secondary causes are acquired or iatrogenic, often resulting from trauma, surgery, or other hip pathologies:
1. Slipped Capital Femoral Epiphysis (SCFE)
- Alters the femoral head-neck junction.
- Increases risk of cam-type impingement.
2. Legg-Calvé-Perthes Disease
- Leads to femoral head deformity and joint incongruity.
3. Developmental Dysplasia of the Hip (DDH)
- Surgical overcorrection can result in pincer-type morphology.
4. Post-Traumatic Deformities
- Malunion of femoral neck or acetabular fractures.
5. Surgical Overcorrection
- Procedures like periacetabular osteotomy may inadvertently create impingement.
6. Acetabular Retroversion
- Can be congenital or acquired, leading to anterior overcoverage.
⚠️ Symptoms of Femoroacetabular Impingement
- Deep groin pain, especially during hip flexion or rotation.
- Clicking, catching, or locking sensations.
- Decreased range of motion.
- Pain during prolonged sitting, squatting, or stair climbing.
🧪 Diagnosis of FAI Syndrome
Diagnosis is based on a triad:
- Symptoms: Pain, stiffness, functional limitations.
- Clinical Tests: Positive FADIR (Flexion-Adduction-Internal Rotation) test.
- Imaging: X-rays, MRI, or CT scans showing cam/pincer morphology.
🏃♂️ Physiotherapy Management of Femoroacetabular Impingement
Physiotherapy is the first-line conservative treatment for FAI. It focuses on improving joint mechanics, reducing pain, and restoring function.
🔹 1. Patient Education and Activity Modification
- Avoid deep squats, lunges, and prolonged sitting.
- Modify sports or occupational activities that provoke symptoms.
🔹 2. Pain Management
- Use of NSAIDs (as prescribed).
- Ice or heat therapy for symptom relief.
🔹 3. Mobility and Flexibility Training
- Gentle stretching of hip flexors, adductors, and external rotators.
- Joint mobilizations to improve capsular flexibility.
🔹 4. Strengthening Exercises
- Focus on gluteus medius, gluteus maximus, and core stabilizers.
- Begin with non-weight-bearing exercises (e.g., bridges, clamshells).
- Progress to functional closed-chain exercises (e.g., step-ups, mini-squats).
🔹 5. Neuromuscular Control and Postural Training
- Emphasize lumbo-pelvic stability.
- Correct faulty movement patterns (e.g., Trendelenburg gait).
🔹 6. Proprioception and Balance Training
- Single-leg stance, wobble board, and dynamic balance drills.
🔹 7. Return-to-Activity Protocol
- Gradual reintroduction of sport-specific drills.
- Monitor for pain or compensatory movement patterns.
📌 Note: A structured rehab program should last at least 12 weeks before considering surgical options.
🛠️ When to Consider Surgical Referral
Surgery may be indicated if:
- Symptoms persist despite 3–6 months of physiotherapy.
- Imaging confirms significant structural abnormalities.
- There is labral tearing or cartilage damage.
Hip arthroscopy is the most common surgical intervention, aimed at reshaping the femoral head or acetabulum and repairing soft tissue damage.
MCQ –
A 40-year-old male patient presents with insidious onset of deep groin pain that worsens with prolonged sitting, stair climbing, and squatting. On examination, FADIR test is positive.
Which of the following physiotherapy interventions is MOST appropriate in the initial stage of rehabilitation?
A. Passive stretching of hip flexors and adductors
B. Deep tissue release over greater trochanter
C. Core and pelvic stabilization exercises with activity modification
D. Progressive resisted abduction exercises in full hip flexion
Answer : Option C
Explanation – In the initial phase, the focus should be on:
Reducing impingement through activity modification
Improving core and pelvic control to reduce abnormal joint loading
Stretching or resisted exercises in provocative positions can worsen symptoms initially
🧩 Final Thoughts
Femoroacetabular Impingement is a complex but manageable condition. Early diagnosis and a tailored physiotherapy program can significantly improve outcomes and delay or prevent the onset of hip osteoarthritis. At Myokin PhysioAcademy, we emphasize evidence-based rehabilitation strategies to empower clinicians and patients alike.
Reference –
https://www.google.com/url?sa=i&url=https%3A%2F%2Fportmelbournephysio.com.au%2Ffemoracetabular-impingement-syndrome-fai%2F&psig=AOvVaw2MnfhGGUBjzRQsdLX9qMIs&ust=1751700843117000&source=images&cd=vfe&opi=89978449&ved=0CBcQjhxqFwoTCKjtrtHYoo4DFQAAAAAdAAAAABAE
austreliansportsphysio.com
